Haemorrhoids are swollen veins in the lower rectum and anus. They are often caused by straining to have a bowel movement or by pregnancy. They can be a temporary condition that goes away without treatment, or a long-term (chronic) problem.
Haemorrhoids are a common condition that affects many people at some point in their lives. In fact, about half of all people have haemorrhoids by the age of 50, and about a third of adults have them by the age of 75. Haemorrhoids can cause pain, itching and bleeding in the anal area.
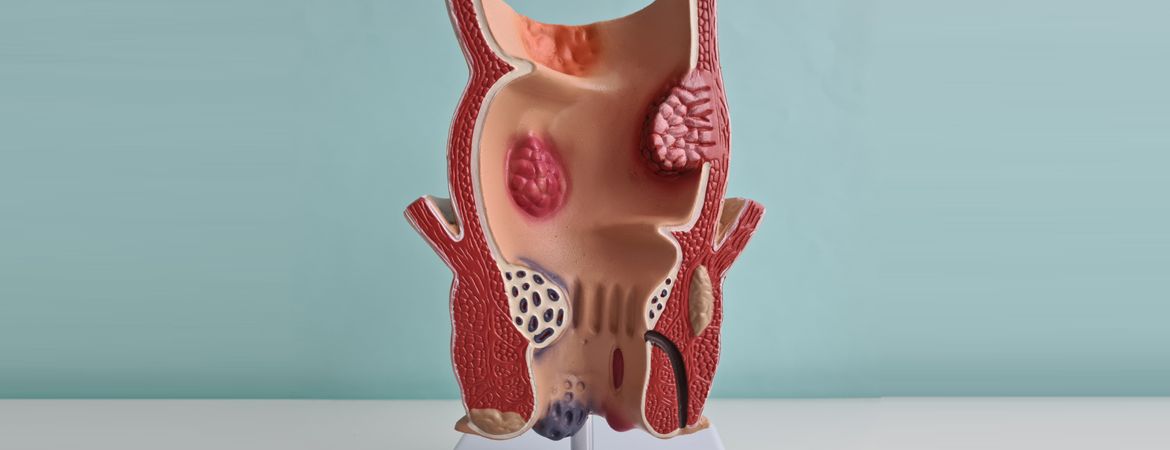
Haemorrhoids can develop inside the rectum (internal haemorrhoids) or outside (external haemorrhoids). Internal haemorrhoids usually cause no symptoms and are not visible. The most common symptom is bleeding during bowel movements – not necessarily every time you go to the toilet, but often enough to be embarrassing.
External haemorrhoids sometimes become inflamed and painful, but are not always visible until they swell or bleed. External haemorrhoids rarely bleed, unless they burst, which can cause considerable pain and discomfort.
WHAT ARE THE SYMPTOMS OF HAEMORRHOIDS?
The symptoms of haemorrhoids are as follows:
- Bleeding from the rectum.
- Painful swelling of the anus.
- Itching and irritation around the rectum.
- Bright red blood on the toilet paper after a bowel movement.
- Painful and sometimes difficult bowel movements.
In some cases, however, haemorrhoids can cause them to prolapse. Haemorrhoidal prolapse is when haemorrhoidal tissue protrudes from the anus. It is common in people with chronic constipation and diarrhoea, and in pregnant women.
Medical treatment for haemorrhoids varies depending on the stage of the condition. In the early stages, when there is no bleeding or discomfort, haemorrhoid creams may be used to shrink them. If they do not respond to this treatment, surgery may be needed to remove them.

CAUSES OF HAEMORRHOIDS
- Family history:
If your parents or other close family members have had haemorrhoids, you’re more likely to get them.
- Pregnancy:
During pregnancy, many women develop haemorrhoids due to increased pressure on the veins in and around the anus. This is because the growing uterus puts pressure on the veins in and around the rectum.
- Constipation:
Constipation can lead to straining to have a bowel movement, which can cause haemorrhoids to appear and make existing haemorrhoids worse, especially if they are already in your body and you don’t know it (silent). Straining to have a bowel movement can also cause anal fissures, which are small tears in the skin around the anus, and rectal prolapse (prolapse means that something falls out of its normal position).
- Lack of exercise:
Lack of exercise can also lead to constipation and straining to have a bowel movement, which can aggravate existing haemorrhoids and cause bleeding in other parts of the colon, such as the ascending colon, part of the large or small intestine.
HOW CAN HAEMORRHOIDS BE PREVENTED?
There are a number of things you can do to prevent haemorrhoids:
Eat a diet high in fibre: Fibre helps soften stools so that they pass more easily through the large intestine. Hard stools can lead to constipation and straining, both of which increase the risk of haemorrhoids. If you get at least 25 grams of fibre a day, whether from food or supplements, you’ll probably find that your stools are softer and easier to pass.
Avoid constipation by eating plenty of fibre and drinking plenty of water. Constipation can lead to increased pressure in the colon and rectum, which can promote the development of haemorrhoids. If you are having trouble having regular bowel movements, try increasing your fibre intake and drinking more water throughout the day; this is usually enough to solve constipation problems for most people. If these measures don’t work, or if the problem persists, talk to your doctor about treating constipation or other digestive problems that may be contributing to haemorrhoids.
Don’t strain to have a bowel movement; use a suppository (medicine) if you can’t get to the toilet quickly enough after the urge to have a bowel movement.

HAEMORRHOIDS IN PREGNANCY
Haemorrhoids during pregnancy are very common, especially in the third trimester. This is due to increased pressure from the growing baby on the pelvic veins, which can lead to the appearance of haemorrhoids.
Haemorrhoids during pregnancy can also be caused by constipation, straining to pass stools and hormonal changes that affect blood circulation. Haemorrhoids are usually painless, but can sometimes bleed or cause itching or discomfort.
Haemorrhoids in pregnancy are a medical condition that should be treated in consultation with your doctor. Pregnancy haemorrhoids can be treated with over-the-counter medicines such as tampons, ointments and witch hazel creams.
WHAT ARE THE TREATMENTS FOR HAEMORRHOIDS?
If you have mild haemorrhoids, you can try home remedies such as warm baths or witch hazel packs to relieve the pain and itching. You can also use softer toilet paper and avoid constipation by drinking plenty of water and eating fibre-rich foods such as fruit, vegetables and wholegrain cereals.
If your symptoms persist, your doctor may recommend medication or other treatments, depending on the severity of your haemorrhoids. The most common options are
Over-the-counter creams containing hydrocortisone (a steroid) or lidocaine (an anaesthetic). These creams can reduce the itching and swelling caused by haemorrhoids.
Rubber band ligation – A small rubber band is placed around the base of an external haemorrhoid to cut off its blood supply and cause it to shrink over time (like a varicose vein). This procedure is often done in an office under local anaesthetic. It is generally effective in treating small external haemorrhoids.

