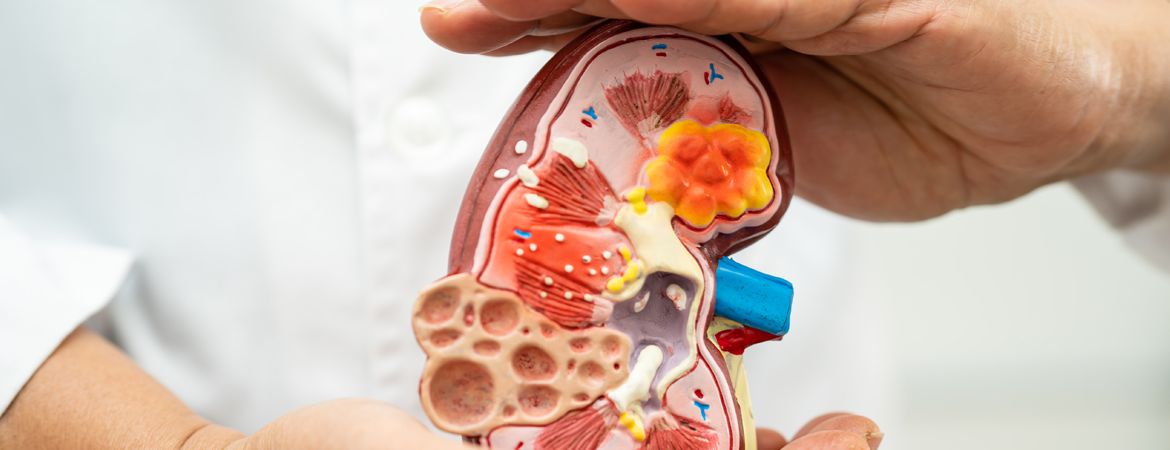
The Nephrology and Dialysis department treats all kidney diseases and conditions associated with chronic kidney disease.
DIABETIC NEPHROPATHY AND RENAL COMPLICATIONS OF OBESITY
Diabetic nephropathy, also known as diabetic kidney disease, is a progressive kidney disease that affects many people with diabetes (a condition treated in our Nephrology and Dialysis department).
It leads to reduced kidney function and increased levels of creatinine in the blood. The renal complications of obesity are due to obesity-induced hyperinsulinism (excessive production of insulin by the body) and consequently insulin resistance, which poses new problems for obese patients.

VASCULAR NEPHROPATHIES
Vascular nephropathies are a group of kidney diseases related to high blood pressure (hypertension).
The blood vessels that supply the kidneys are damaged; causing bleeding and scarring that can eventually lead to permanent kidney damage.
This condition can lead to kidney failure, which can only be reversed by lifelong dialysis or a kidney transplant.
The most common forms of vascular nephropathy are
Hypertensive nephrosclerosis:
This is caused by high blood pressure (hypertension). Over time, high blood pressure damages the small arteries of the kidney, causing them to shrink or collapse. This can reduce blood flow to the kidneys and eventually lead to kidney failure.
Polycystic kidney disease:
In this condition, cysts develop over time along the length of a person’s kidneys, causing scarring and damage to normal kidney tissue. As the cysts grow, they can begin to block normal blood flow to the kidneys, which can eventually lead to kidney failure if left untreated.
KIDNEY STONES
Renal lithiasis (a condition treated in our Nephrology and Dialysis department) is defined as the presence of a stone in the kidney, with or without significant symptoms.
Renal lithiasis can be caused by spontaneous passage of kidney stones, recurrent urinary tract infections due to bacteria that produce kidney stones (such as staphylococci), or other urinary tract diseases that lead to the formation of granular flow and stone formation.
Symptoms of kidney stones can include:
- Painful urination
- Bloody urine
- Urinating more often than usual
Doctors can diagnose kidney stones using ultrasound, CT or intravenous pyelography (IVP). These tests help the doctor to determine the type of stone you have and measure its size, so they can decide on an appropriate treatment plan.


DIALYSIS
Dialysis (provided by our Nephrology and Dialysis department) is a medical procedure used to remove waste products, excess fluid and extra nutrients from the blood when the kidneys are unable to do so.
Dialysis is used when the kidneys are severely damaged or have stopped working altogether (end-stage renal disease).
There are two types of dialysis: haemodialysis and peritoneal dialysis.
Haemodialysis uses a machine that filters blood outside your body and returns the cleaned one to you in the form of a dialysed solution. The machine is called a dialyser and consists of two parts: a filter that removes waste products and a tube that carries the blood through the filter before returning it to your body. The process takes about 4 hours per session, 3 times a week on average.
Peritoneal dialysis removes waste products from your body using an ultrafiltration membrane inside an abdominal bag called a peritoneal dialysis catheter (PDC). Waste is removed by applying positive pressure to the abdomen, causing it to pass through the PDC membrane into the abdomen, where it is then flushed down the toilet after each treatment.
Our nephrology and dialysis specialists know how to manage this type of condition and provide the best possible care.
WHAT IS AN ARTERIOVENOUS FISTULA?
Arteriovenous fistulas (AVFs) are the most common vascular access for haemodialysis. They are surgically created by connecting an artery and a vein to allow blood to flow in and out of a diseased kidney.
The AVF is created between the radial artery and the cephalic vein, which are lateral branches of the brachial and axillary arteries, respectively. The radial artery is usually chosen because its pulse is less prominent than that of the brachial artery.
An AVF is usually created by joining two separate vessels in an end-to-end anastomosis, where one vessel is sutured to another to create a continuous vein or artery. This type of procedure is called an anastomosis. The surgeon must make sure that there are no leaks or blood clots in the new AVF during this process.
WHAT IS A HAEMODIALYSIS CATHETER?
A haemodialysis catheter is a long, flexible tube that is inserted into the body to remove waste products from the blood. The catheter has two openings that allow blood to flow out of the body and into a dialysis machine. This process removes excess waste from the blood. It also takes place outside the body, so no surgery is required.
Haemodialysis can be used to treat a wide range of conditions, including chronic kidney failure, heart failure and high blood pressure. It can also be used as an emergency treatment for people who have had a stroke or heart attack.
People undergoing haemodialysis usually have one or more dialysis sessions a week at a clinic or hospital where they live. Before each session, a doctor inserts a catheter into an artery in the arm or leg to make it easier to access the blood vessels during treatment.
WHY SHOULD I visit A NEPHROLOGIST?
A nephrologist is a doctor who specialises in caring for people with kidney disease. Nephrologists have completed at least five years of medical school, followed by three to seven years of training in internal medicine.
A nephrologist is a specialist in kidney disease. Nephrology is one of the most advanced medical specialties today.
Nephrology covers all aspects of kidney disease, from prevention and screening to treatment and management. It also includes the related areas of hypertension (high blood pressure) and electrolyte imbalances (such as low potassium levels).
In addition to treating patients, nephrologists work with other members of the healthcare team to develop new therapeutic approaches to reduce complications and improve the quality of life for people with kidney disease.
Nephrologists are trained to treat a wide range of kidney diseases and disorders, including:
– Chronic kidney disease
– Kidney stones
– Acute kidney failure
WHAT TESTS DOES A NEPHROLOGIST CARRY OUT?
Nephrologists carry out a wide range of tests to diagnose and monitor kidney disease. They may also use tests to diagnose and monitor other conditions that affect the kidneys, such as heart disease.
Here are some of the more common tests:
Blood tests: To find out if there is a problem with your kidneys, blood samples are taken for analysis. The samples may be sent to a laboratory for analysis or processed by a machine in the doctor’s office. The results of these tests are used to diagnose kidney problems and assess their severity.
Kidney function tests: These tests assess how well the kidneys are working by measuring the amount of waste they remove from the blood. They include urine volume, urine specific gravity and creatinine clearance (the amount of creatinine removed from the blood).
Serum creatinine test: This test measures the amount of creatinine in the blood at a given time. Creatinine is broken down by the kidneys into urea, which is excreted in the urine. As kidney function declines, less urea is produced and less creatinine is found in the urine.
We present to you some articles relating to pathologies treated in our Mediterranean clinic, with an effective and efficient medical and paramedical team.
A urinary tract infection (UTI) is an infection of the urinary tract, including the kidneys, ureters and bladder.
A UTI causes symptoms such as pain when urinating, frequent urination, and cloudy or foul-smelling urine. In more serious cases, UTIs can cause blood in the urine and fever.
A UTI is usually caused by bacteria entering the urethra and travelling up to the bladder. This can happen if you wipe from back to front after going to the toilet, if you have sex without using a condom, or if you leave a wet swimsuit in for a long time without drying it properly.
Symptoms of a urinary tract infection include:
- Pain when passing water (dysuria)
- Frequent need to urinate (frequency)
- Cloudy or foul-smelling urine
Pyelonephritis is a bacterial infection of the kidneys. Although it can affect any part of the urinary tract, pyelonephritis usually affects the upper part of the kidney. This is called pyelitis.
Pyelonephritis causes pain and tenderness in the side or back. You may also have a fever and chills.
Pyelonephritis is usually caused by bacteria that enter the urinary tract through the genitals or anus. But some cases are caused by bacteria that have spread from an existing infection elsewhere in the body, such as a bladder infection or ear infection (otitis media).
A urine test can confirm that you have pyelonephritis. Treatment depends on the severity of your symptoms, your health and whether you have other medical conditions.
The signs and symptoms of pyelonephritis include:
- Fever
- chills
- Tremors (convulsions)
- Nausea or vomiting
- Stomach pain, cramping or tenderness (abdominal pain) in the lower right part of your abdomen (hypochondrium)
- Painful urination, which may be difficult at first but gets easier as you go – this means you are passing less urine than usual because your kidneys are inflamed (oliguria).
- Blood in the urine (haematuria)
Definition of renal colic
Renal colic is a condition characterised by sudden, severe pain in the lower back and abdomen, radiating into the groin. The pain is provoked by urination or other forms of abdominal pressure (such as coughing). It may be accompanied by nausea and vomiting.
The pain can last from a few minutes to several hours. Renal colic is also known as kidney stone disease.
Symptoms of renal colic
The following symptoms may indicate that you have renal colic:
- Pain in your lower back or abdomen
- Nausea and vomiting
- Fever
- A feeling of heaviness on one side of the abdomen
Rhabdomyolysis is a condition in which damaged muscle tissue leaks into the bloodstream, causing kidney damage. Rhabdomyolysis can be caused by crush injuries, electric shock, drug use and other traumatic events.
Rhabdomyolysis can also be caused by prolonged exercise and exposure to heat. If the body is unable to cool itself properly by sweating, muscles can begin to break down.
In addition to kidney failure, rhabdomyolysis can cause permanent damage to other organs such as the heart, lungs and brain.
You ask, our teams answer.
F.A.Q
Nephrology is the medical speciality that deals with the kidneys and their diseases. Nephrologists assess and treat diseases of the kidneys, ureters and bladder. They also study the effects of kidney disease on other body systems.
Nephrologists usually provide a long-term care for patients with chronic kidney disease (CKD). They also treat acute kidney injury, which occurs when a sudden loss of kidney function leads to a build-up of toxins in the body. Nephrologists work with other specialists such as nephrological surgeons, paediatric nephrologists, dialysis nurses and haemodialysis technicians to provide optimal care for patients with kidney disease.
Nephrology requires a wide range of knowledge and skills to treat different types of kidney problems. Treatment options may include drugs, surgery or dialysis. Nephrologists usually have hospital privileges at several facilities, which allows them to spend more time with their patients during treatment procedures such as dialysis sessions or surgical recovery.
Diabetic nephropathy is a condition in which the kidneys are damaged by high blood sugar (glucose) levels. The two main types of diabetic nephropathy are diabetic nephropathy and diabetic renal tubular acidosis.
Diabetic nephropathy occurs when high levels of glucose damage the small blood vessels (capillaries) that carry blood to the kidneys. This process causes scarring and thickening of these capillaries, reducing blood flow to the kidneys. As the kidneys lose their ability to filter waste from the body, the urine becomes more concentrated with waste. This leads to other symptoms such as increased thirst (polydipsia), increased urination (polyuria) and tiredness.
Diabetic renal tubular acidosis occurs when high levels of glucose upset the body’s normal acid-base balance. Acid-base balance is important for many functions, including digestion and absorption of nutrients from food and fluids in your body.
If you have any signs or symptoms of diabetic kidney disease, talk to your doctor immediately to see if treatment is needed.
Kidney stones are hard deposits that form in the kidneys. They are made up of substances in the urine that are too solid to pass through the urinary tract. Kidney stones are not usually serious, but they can be painful and lead to a long-term health problems.
Kidney stones form when chemicals in the urine concentrate to form crystals that clump together to form a stone. Most kidney stones contain calcium, but other substances such as uric acid, cystine and struvite may also be involved. The size and composition of these stones vary depending on their location in the kidney.
Urine naturally contains substances that help prevent the formation of kidney stones. If these substances are not present in sufficient quantities, certain minerals can crystallise out of solution and form small crystals or stones.
The formation of small kidney stones is quite common – over 10% of men and 5% of women will have at least one in their lifetime. In most cases, these small stones pass without treatment within a few days or weeks. However, larger stones may require medical intervention to prevent serious complications later on.
Obesity is a chronic condition in which excess body fat has accumulated to the point where it is adversely affecting health. The level of body fat in relation to height, gender and age is used to define obesity in adults.
Obesity is associated with a number of life-threatening comorbidities, including cardiovascular disease and diabetes mellitus. Obesity is also associated with increased morbidity and mortality from malignant neoplasms, respiratory diseases and musculoskeletal disorders. Some complications are directly attributable to obesity, while others are related to its comorbidities.
Renal complications of obesity include:
– Hypertension (high blood pressure) and hypercholesterolaemia (high cholesterol) – risk factors for kidney disease
Diabetes mellitus – also known as diabetic nephropathy or diabetic kidney disease, this complication affects both type 1 and type 2 diabetics who are overweight or obese. It usually develops over time, but in some cases it can happen quickly, especially if you get an infection such as pneumonia or a urinary tract infection (UTI). Diabetic nephropathy can lead to acute kidney failure requiring dialysis or transplantation; it also increases the risk of cardiovascular disease, including stroke.