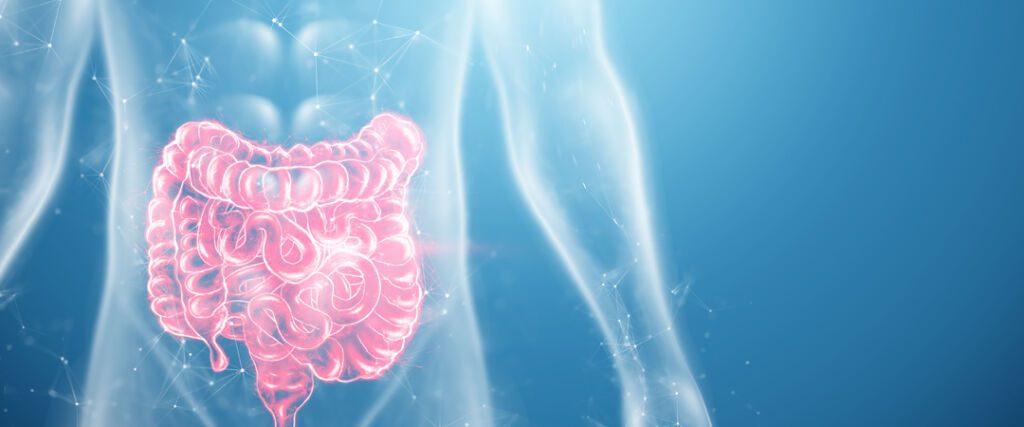
Bowel cancer is one of the most common cancers in humans. It ranks behind prostate and lung cancer in men and just behind breast cancer in women. On average, bowel cancer strikes people between the ages of 70 and 75. It affects the cells in the inner lining of the colon. If detected early, bowel cancer is preventable.
DEFINITION OF BOWEL CANCER:
Bowel cancer is a cancer of the large intestine. It is mainly found at the end of the digestive tract, but can also affect the inner lining of the colon.
It is a disease of the cells in the rectum that multiply abnormally to form a cancerous tumour. There are around 1.5 million cases worldwide each year. It is on the increase.
Bowel cancer is initially benign and is called a polyp. Over the years it can develop into a malignant tumour. Survival rates vary widely. However, the disease can be treated and cured in up to 90% of cases, depending on its severity.
CAUSES OF BOWEL CANCER
No study has been able to identify the actual causes of bowel cancer. However, several risk factors have been identified. Age is the most important risk factor for bowel cancer. Most cases occur in people over the age of 50.
Family and medical history also increase the risk of developing bowel cancer. This is the case, for example, for people with chronic inflammatory bowel disease or Lynch syndrome. A screening test is needed.
Preventing bowel cancer also involves lifestyle choices. You need to watch what you eat and take regular exercise.
Bowel cancer is a disease in which malignant (cancerous) tumours develop in the colon or rectum. These tumours can be benign (non-cancerous) or malignant.
The different stages of bowel cancer are as follows/
Stage I: The tumour is small and confined to the inside wall of the colon or rectum. It has not spread to other parts of the body.
Stage II: The tumour has grown through the lining and into nearby tissues, such as muscle or fat. It has not spread to the lymph nodes or other parts of the body. This stage is also known as Dukes’ colon cancer A, because it is classified according to a system known as the Duke Classification, or stage A2 in the American Joint Committee on Cancer staging system.
Stage III: The tumour has penetrated the wall of the colon or rectum and reached nearby lymph nodes (lymph nodes are part of the immune system). It may have spread beyond these lymph nodes but has not reached nearby organs such as the liver, lungs or bowel. This stage is also known as Duke’s stage B bowel cancer, because it is graded according to a system called the Duke Classification, or stage B.
HOW BOWEL CANCER SPREADS
Bowel cancer starts in the colon or rectum and spreads to other organs through the lymphatic system or bloodstream. To find out more about how bowel cancer spreads, including its early stages and symptoms, read our cancer treatment guide.
LYMPH NODE METASTASES
In around 30% of people with bowel cancer, the disease spreads to nearby lymph nodes – small structures in your body that are part of your immune system. Lymph nodes are found all over the body, usually near blood vessels. They filter out germs and other substances that enter the body through the mouth, nose, skin or vagina.
If your doctor finds evidence of lymph node involvement on a CT scan or biopsy sample, he or she may recommend that you have surgery to remove these lymph nodes. This is called a ‘lymphadenectomy’. If all the suspicious lymph nodes are not removed during surgery, imaging tests such as CT or PET scans may be used to check whether they are still active.
Bowel cancer does not cause any major symptoms at first because the disease is still very small. It can only be detected by screening, which is strongly recommended for people over 50. As non-cancerous polyps develop, symptoms appear.
The most common are abdominal pain, bowel problems and blood in the stool. The latter can often be associated with haemorrhoids. Some patients suffer from anaemia, persistent diarrhoea, swollen lymph nodes, etc.
Bowel cancer can be asymptomatic, but if it’s not detected early, problems can spread to other organs.
Treatment for bowel cancer varies depending on the stage of the disease, the size of the affected cells and their location. However, patients who receive the right treatment can have good outcomes and a better chance of recovery.
There are a number of common treatments for bowel cancer. Surgery removes the affected part of the bowel. Chemotherapy is used to kill cancer cells. Before surgery, radiotherapy is used to burn the malignant cells and reduce the size of the tumour. Targeted therapies are also available for more specific situations.
People with certain risk factors for bowel cancer should be screened regularly. If you have an average risk of bowel cancer, you don’t need to be screened before the age of 50. Your doctor will decide when to start screening based on your personal history.
The two most common tests for bowel cancer screening are:
- Colonoscopy, where the colon and rectum are examined using a flexible tube called a colonoscope.
- Fecal occult blood test (FOBT) or faecal immunochemical test (FIT), which detects the presence of hidden blood in stools.
Bowel cancer surgery, also known as bowel resection, is the removal of all or part of the large bowel. Bowel cancer surgery may be performed for a number of reasons, including:
- To remove cancerous tissue from the colon
- To treat colitis, a condition that causes irritation and inflammation of the colon
- To treat inflammatory bowel disease (IBD), which includes ulcerative colitis and Crohn’s disease.
- To treat complications of diverticulitis, an infection of small pouches in the wall of the colon.
Bowel cancer surgery can be done either open or laparoscopically. Open surgery requires a large incision in the abdomen to gain access and remove tumours or abnormalities. The surgeon then uses stitches or staples to close the incision. Laparoscopic surgery uses small incisions through which surgical instruments are passed into the abdominal cavity to remove cancerous tumours. There are several types of laparoscopic surgery: Minimally invasive surgery (MIS), robotic-assisted MIS (R-MIS) and da Vinci robotic-assisted MIS.
After surgery, you may have an ileostomy or colostomy. An ileostomy is when the large bowel ends in the skin rather than in the rectum. A colostomy is when the large bowel ends in an opening near the skin instead of joining the rectum.
There are some things you’ll need to do after surgery to help prevent complications:
Follow your doctor’s instructions about taking medicines and supplements during chemotherapy or radiotherapy. These medicines can affect the quality of your healing after surgery.
Eat small, frequent meals rather than large ones. This will help prevent nausea and vomiting, which can lead to dehydration and anaemia from blood loss.
Take antibiotics before dental or other procedures that require needles, if necessary, to prevent infection of the surgical site (wound).
You ask, our teams answer.
F.A.Q
A genetic predisposition to colorectal cancer is a condition in which an individual has an increased risk of developing colorectal cancer. This increased risk may be due to the inheritance of certain genetic mutations.
Colorectal cancer is the third most common cancer worldwide and the second most common cause of cancer death in developed countries . Approximately 1 million new cases of colorectal cancer are diagnosed each year worldwide. The majority of colorectal cancers occur sporadically, but around 5-10% of people with colorectal cancer have a family history of the disease. A family history of bowel cancer significantly increases the risk of developing bowel cancer.
Genetic predisposition to bowel cancer is determined by certain genetic mutations that increase the likelihood of developing the disease. Genetic tests can determine whether a person carries these mutations. These tests include:
Gene sequencing: analysis of all exons and introns (protein-coding regions) of a gene to detect any changes that may lead to abnormal function or expression .
Mutation analysis: analysis of the entire coding region and regulatory regions (DNA outside the protein-coding regions that controls the amount of protein produced).
The effects of an unhealthy diet on bowel cancer can be devastating. Medical treatment for bowel cancer includes surgery, chemotherapy, radiotherapy and immunotherapy. A healthy diet is important throughout the course of the disease. The consequences of a poor diet are an increased risk of developing other cancers, such as breast, prostate and ovarian cancer. Bowel cancer survivors have a higher risk of heart disease and diabetes than the general population. Cardiovascular disease is more common in people who have had chemotherapy or radiotherapy than in those who have not.
Risk factors associated with developing bowel cancer include:
Age: People over 50 have a higher risk of bowel cancer than younger people. Men also have a higher incidence rate than women until the age of 70 or 80, when the rates between men and women equalise.
Family history: A family history of bowel cancer increases the risk of developing it because certain genes increase susceptibility to this type of cancer. If you have two close relatives (a parent or sibling) diagnosed with bowel cancer before the age of 60, your risk increases by 2% per year during that period.
If you have a polyp, the risk of it developing into cancer is low. However, certain factors can increase this risk.
The most important factor is location. Polyps in the rectum or lower bowel are more likely to become cancerous than those in the upper bowel. This is because there are more stem cells in the upper bowel, which means they are more likely to develop into cancer cells.
What’s more, certain types of polyps are more likely to become cancerous than others:
- Adenomatous polyps have a high risk of becoming cancerous and should be removed immediately. They are usually found in people who have already had bowel cancer and have been diagnosed with adenomatous polyps in the colon.
- Hyperplastic polyps are also at high risk of becoming cancerous and should be removed immediately if they are found during screening or if they cause symptoms such as bleeding or pain. These growths are usually found in people who have no family history of bowel cancer, but whose parents have had inflammatory bowel disease (IBD), such as Crohn’s disease or ulcerative colitis.
A digestive stoma is a surgical opening in the digestive tract that allows waste to pass out of the body.
A stoma is a hole or opening in your abdomen. It can be created by surgery, for example if the bowel is removed because of cancer or other illness. A stoma can also be created during other types of surgery, such as when part of the stomach is removed because of ulcers or other conditions.
The opening of a stoma is usually covered by a pouch system that collects and holds stool until it is passed out of the body. The device has a one-way valve that prevents air from entering the body and helps to prevent blockages in the digestive tract. The pouch system also includes a collection pouch that holds stool until you empty it each day.
You’ll learn how to care for your ostomy during your hospital stay after surgery, at home during follow-up visits with our nurses, and throughout your life as an ostomy patient.